When the Secretary for U.S. Department of Health and Human Services first declared a nationwide public health emergency (PHE) in April 2020, a flurry of telehealth policy changes followed.
At the peak of the pandemic, the federal government announced these changes on a near-daily basis: waivers and factsheets and FAQs (oh my!).
Many of these policies were created specifically to expand telehealth adoption and access. For instance, community-based providers — like health centers and rural health clinics — could now see patients from home. Doctors could practice more easily across state lines. Patients could use everyday technology, like WhatsApp and iMessage, to connect with providers during the emergency. Some of these initial policy changes were explicitly temporary and could change again.
Perhaps most significantly, Medicare announced telehealth coverage for 144 additional medical services, matching payment rates (“payment parity”) for in-person care during the (ongoing) emergency period.
Because telehealth reimbursements are often much lower than the same service provided in-person, payment parity’s an important incentive for medical practices to make telehealth available to more patients. That incentive has downstream public health benefits — with virtual options for care, patients can worry less about spreading or contracting COVID-19 while visiting the doctor.
And while payment parity’s a temporary measure during COVID-19, Medicare’s 2021 fee schedule included the most significant changes to medical codes in 30 years, extending or making permanent some of the temporary rules.
A lot of this we learned from trial and error. It’s so hard.
Medical biller with 13-years of experience
Billing challenges on the ground
Billing and coding changes weren’t just significant from a policy standpoint, though. Throughout the pandemic, medical billers and coders — the administrative staff responsible for billing patients and submitting claims for reimbursement — have had to completely revamp the way they code, document, and bill for telehealth.
I learned about some of these challenges while interviewing clinical staff in the field.
A biller with 13 years of experience working at a small, federally-funded rural hospital in California, talked about difficulties keeping up with new rules and regulations, particularly in the early months of the pandemic, when reimbursement rules were nearly constantly in flux. “You can get one person to process [a claim] one way, and the next person will process it another way. It’s all up to interpretation. A lot of this we learned from trial and error. It’s so hard.”
Sometimes a new rule would come out that applied to backdated claims, requiring staff to re-code. Sometimes those claims would get denied anyway, even after trying to carefully follow the new policies.
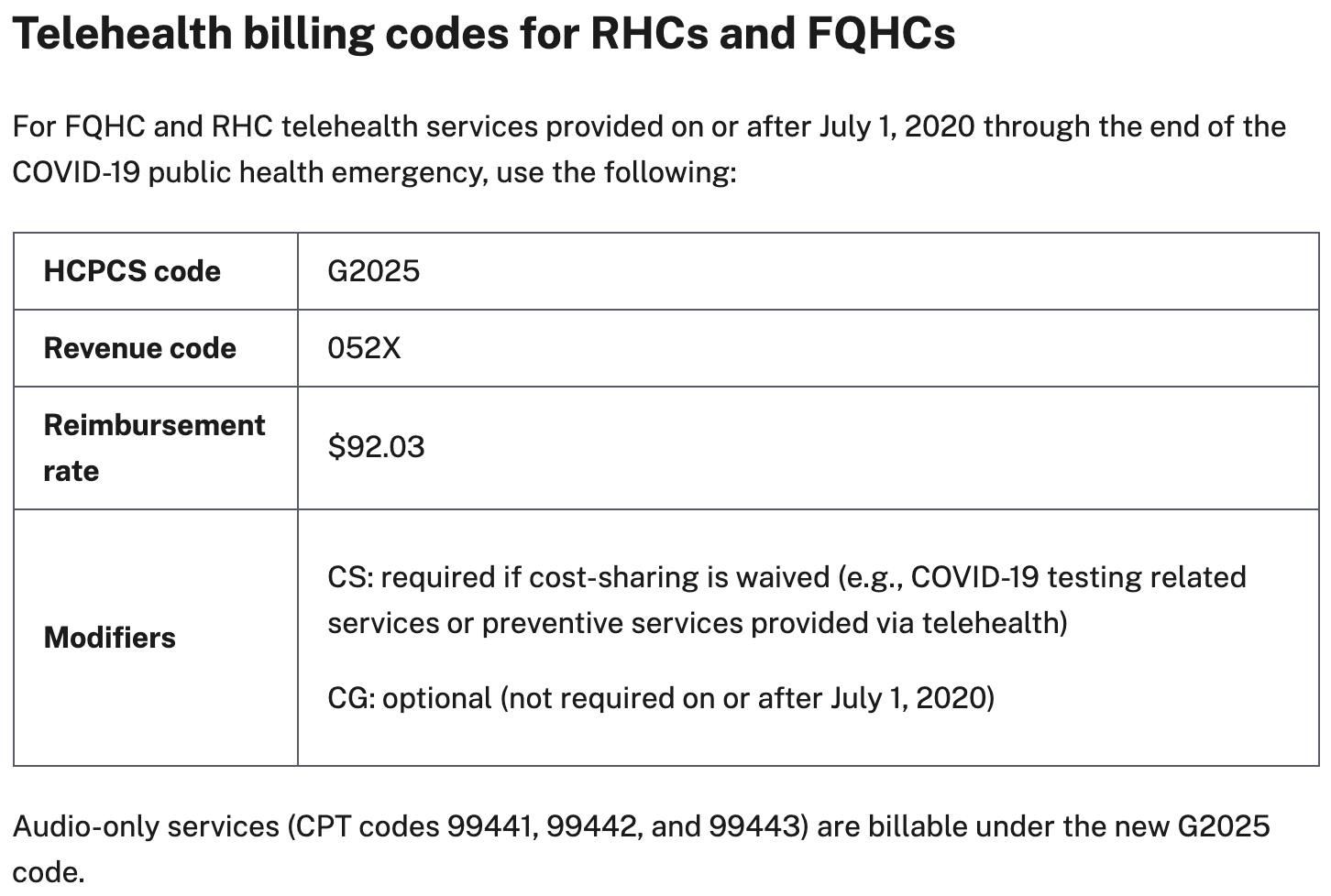
Another challenge: Guidance for safety net providers, like rural health clinics and community health centers, was often lumped together with other providers, even when they had unique rules and regulations to follow. Interviewees at these clinics described digging through lengthy documents to find information specific to their needs — and, as one biller put it: “When you get to digging that’s when you get confused.”
The lack of consolidated, user-friendly policy guidelines made understanding and implementing the new rules and regulations tricky across the board. Billers and coders relied on Medicare to understand what policies had changed and how to implement them, but there was no “single source of truth” for information. When documentation did exist, access was cumbersome — for instance, 100+ page PDFs or a billing codes list you must download to read.
There are massive consequences at stake. When providers can’t get reimbursed for their services, they risk shutting down. For the public — particularly vulnerable communities in hard-hit areas with very few options — this could mean losing access to healthcare during a pandemic, even when the policies should allow for much more flexible access than ever before.
Making policy information more human friendly
The interviews with telehealth billing and coding staff left me wondering: How can we communicate vital information to people who need it for their everyday jobs, like medical billers and coders? How might we make it easier for clinical staff to find information relevant to their practice? What if we could distill and “translate” complex guidelines into actionable, accessible, plain language “how-tos”?
Focusing on improvements to the digital delivery of policy information (only one piece of the puzzle!), what if policy guidelines were…
- Accessible directly from the web (without extra barriers like large file downloads)?
- Customized (for example, by provider type), with a clear, authoritative source of truth for each audience?
- Easy to search?
Medicare’s List of Telehealth Services became the only way for billers and coders to find all the billing codes covered during the COVID-19 emergency. The spreadsheet routinely requires updates to align with new billing policies, but it’s burdensome to use. It’s inaccessible directly from the web, requiring a download to view its contents. And the format restricts its usability further because it’s cumbersome to search — coders rarely need the entire universe of codes every time they want to look into coverage. There’s also the possibility that information is out of date, particularly when policies were changing every week.
With difficult-to-use regulatory information in such high demand in the midst of a health crisis (it’s regularly one of the top downloads across all of Health and Human Services), I wondered: What if instead of a download-only spreadsheet, staff could search through Medicare’s list of covered telehealth services directly on the web?
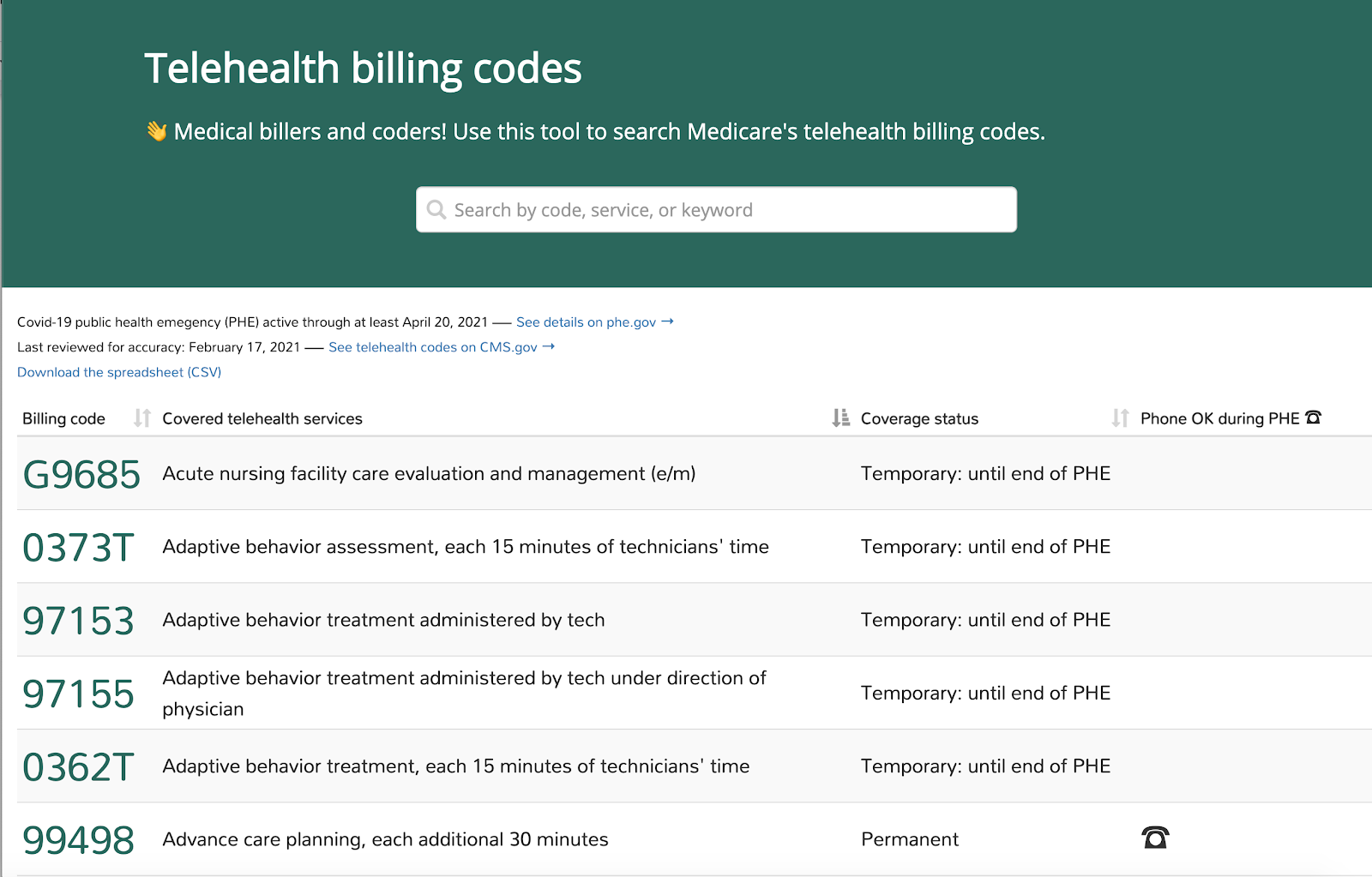
Searchable billing codes prototype I created
And what if Medicare & Medicaid policies were described in plain language and provider-specific?
Screenshot from Telehealth.HHS.gov, a Skylight project built with Health Resources and Services Administration.
Why this matters
Simple changes to how policy information is delivered by the government can improve public health. A new billing code can mean a person with 15 years of experience suddenly has to spend significant time understanding basic requirements — time that’s essential during a national emergency.
The pandemic, and the deluge of regulatory changes that followed (and which continue to evolve), demonstrates how critical it is to think about — and support — behind-the-scenes staff who are directly impacted by these changes.
